A DEXA scan is a comparatively simple process. The treatment that follows is also very simple. All it takes is the time you would probably take to sip a cup of coffee and relish its taste. It is highly recommended if you belong to any of the following groups:
- Middle-aged women >45 years
- Postmenopausal women
- Men >60 years
- Women undergoing tamoxifen treatment
A DEXA scan can help assess your bone health and detect early signs of osteoporosis. This is particularly important for middle-aged women over the age of 45, who should take proactive steps to prevent silent osteoporosis. Due to the loss of estrogen, postmenopausal women are at a higher risk of developing osteoporosis, making DEXA scans a crucial tool for assessing their bone health.
Men over the age of 60 may experience a gradual loss of bone density, putting them at risk of osteoporosis and fractures. For this reason, a DEXA scan is recommended for them. Women taking tamoxifen for breast cancer and at risk of developing osteoporosis should be regularly monitored with bone density scans, including DEXA scans, to assess the effectiveness of treatment and make any necessary adjustments.
In short, DEXA scans can identify individuals at high risk of fractures and allow for appropriate interventions to prevent or treat osteoporosis.
Osteoporosis is a prevalent medical condition characterised by fragile bones, increasing the risk of fractures. This condition predominantly affects older adults and women, with postmenopausal women being particularly susceptible due to declining estrogen levels. In fact, 1 in 5 women ( 20%) and 1 in 20 men (5%) aged 50 and above are affected by osteoporosis, highlighting its widespread impact.
Risk factors for osteoporosis encompass age, family history, low body weight, smoking, and excessive alcohol intake, as well as specific medical conditions like thyroid issues and inflammatory bowel disease. Additionally, sedentary lifestyles, diets deficient in calcium and vitamin D, and prolonged use of medications like corticosteroids can further exacerbate the condition.
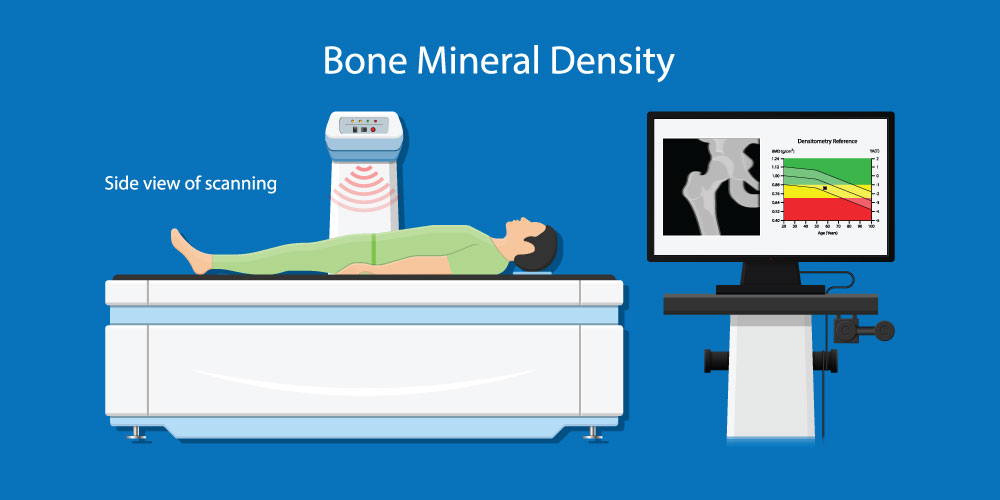
The Dual-Energy X-ray Absorptiometry (DEXA) scan is a widely used and precise bone density test for diagnosing osteoporosis and evaluating an individual's fracture risk. It stands as the most reliable method for assessing bone mineral density.
A DEXA scan employs a minimal amount of low-dose X-ray to assess bone mineral content in targeted areas, typically the hip and spine. This painless, non-invasive procedure can be completed in just a few minutes.
Osteoporosis is very common, and is usually known as the "silent disease." It often presents no symptoms until a fracture occurs, usually in the hip, spine, or wrist. Consequently, screening for osteoporosis is crucial, as it can be challenging to detect in the absence of noticeable symptoms.
Early detection of osteoporosis via bone density testing can identify individuals at risk for fractures, allowing healthcare providers to implement preventative measures. Osteoporosis is a manageable condition, and a healthcare professional can assess an individual's risk factors and tailor an appropriate course of action to their unique circumstances. Prompt diagnosis and intervention often lead to improved outcomes in managing the condition.
A DEXA scan report provides information about bone density and fracture risk and includes several key measurements:
Bone mineral density (BMD) measurement represents the amount of mineral in your bones, reported as grams of mineral per square centimetre of bone. A higher BMD indicates stronger bones, while a lower BMD may indicate weakened bones and an increased risk of fractures.
A T-score compares your BMD to the average BMD of healthy young adults of the same gender. T-scores of -1 or above are considered normal, while those -1 to -2.5 indicate osteopenia ( low bone mass), and those -2.5 or below indicate osteoporosis.
Z-score compares your BMD to that of people your own age and gender and can help your healthcare provider determine whether your bone loss is age-appropriate or may be due to other factors.
Understanding these measurements is important in assessing bone health and identifying potential risks for fractures. It is recommended to discuss the results of the DEXA scan with a healthcare provider to determine the best course of action for maintaining bone health.
Treatment for osteoporosis usually comprises:
- Lifestyle modifications
- Regular exercise
- Calcium and vitamin D-rich diet
- Medication to enhance bone density and minimise fracture risks.
For effective osteoporosis treatment, lifestyle modifications might be insufficient, and medication may be required. Bisphosphonates are frequently prescribed as a primary treatment, while denosumab is another option. Studies highlight the potential for increased spinal fracture risk when medication is discontinued abruptly, emphasising the need for consistent use.
With age, bone breakdown and rebuilding processes naturally occur, but post-menopause, these processes intensify. Osteoporosis medications primarily function by either decelerating bone breakdown or accelerating bone rebuilding. This fortification of bones helps lower fracture risks and enhances bone health. Ultimately, engaging in osteoporosis treatment is a vital step towards better bone health.